 “The business of business is business,” proclaimed Milton Friedman, one of the most famous economists of the 20th century. This catchy phrase makes three key points. Firms ought to be focused on promoting shareholder interest, on making profit, the more the better – but they should do this, one might add, without blatant violation of the law (grey zones are another matter). Moreover, governments, regulators and the general public ought to let firms get on with this job; they should keep legal restraints and regulatory burdens slight and simple so that firms can go about their business with minimal constraints, distractions and friction costs. Finally, firms and economists should prod and lobby officials and the public toward the right – light – approach that gives firms much freedom to prosper.
“The business of business is business,” proclaimed Milton Friedman, one of the most famous economists of the 20th century. This catchy phrase makes three key points. Firms ought to be focused on promoting shareholder interest, on making profit, the more the better – but they should do this, one might add, without blatant violation of the law (grey zones are another matter). Moreover, governments, regulators and the general public ought to let firms get on with this job; they should keep legal restraints and regulatory burdens slight and simple so that firms can go about their business with minimal constraints, distractions and friction costs. Finally, firms and economists should prod and lobby officials and the public toward the right – light – approach that gives firms much freedom to prosper.
Friedman’s view is widely shared among people in the business world, in the financial sector, in economics departments, in politics and in the general public. It resonates with the idea that freedom is good in itself. It also draws support from the thought, powerfully articulated by Bernard Mandeville (1714) and Adam Smith (1776), that the profit motive is a stronger, more reliable source of public benefit than altruistic virtue.
Imagine a pharmaceutical sector that takes Friedman’s mantra to heart, firms that exist in the world as we know it, dependent upon monopoly markups for their earnings and single-mindedly devoted to advancing shareholder interest. How would such – hypothetical – companies respond to something like the COVID-19 outbreak?
Such firms would want to get one or more suitable pharmaceuticals onto the market quickly and then sell such products as profitably as possible, where profit depends on the sales volume and the size of the markup (= unit price minus variable cost of production). Accordingly, such Friedmanian firms would want relevant pharmaceuticals to be in high demand, as measured by the amount of money that solvent buyers are willing to spend, and they would want to appropriate as much of these potential earnings as possible.
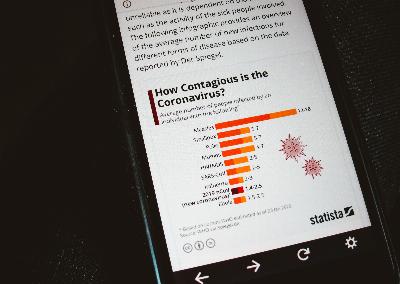
High market demand is driven by need. The need generated by the outbreak of a new disease is greater the more harmful the disease is and the more widely it spreads. If the outbreak becomes a pandemic, then many more people will be and feel at risk, and at greater risk of exposure and infection. Need is increased also when such a pandemic lasts longer and especially when it evolves dangerous new variants that, by requiring additional innovations, open new research and development (R&D) challenges with new profit opportunities.

A Friedmanian firm will therefore want to impede competition and limit supply in order to induce anxious buyers to pay higher prices.
Even if buyers would be prepared to pay a very high price for a product, they will naturally try to obtain it for much less. They will succeed if the market is well supplied by competing sellers. A Friedmanian firm will therefore want to impede competition and limit supply in order to induce anxious buyers to pay higher prices.
Confronted with an infectious disease outbreak, the general public has three key interests:
- that innovators quickly develop or identify pharmaceuticals that can effectively protect individuals from harm and help contain and suppress the disease at the population level,
- that production of such effective pharmaceuticals be rapidly scaled up to meet the global need and
- that supply, as it becomes available, be directed to where it can avert the most harm, taking population effects into account.
How well would Friedmanian firms operating under a monopoly patent regime serve these interests?
Such firms would want;
- to quickly develop new pharmaceuticals that can effectively protect individuals from harm without impeding the proliferation of the disease,
- to scale up production of such new pharmaceuticals judiciously in order to capture market share even while safeguarding proprietary technologies and know-how, avoiding wasteful excess capacity and maintaining a favorable demand-supply imbalance to sustain high prices,
- to prioritize buyers who are offering to pay more and to reject potential buyers who, only marginally profitable, might erode the product price and are more useful spreading and prolonging the epidemic with potential emergence of new disease variants and
- to forestall regulatory interference in, and public awareness of, their profit-maximizing stratagems by making it appear that fighting the disease as effectively as possible is really their most profitable strategy or, more plausibly, that they are wholeheartedly dedicated to this fight, profits be damned.
While actual pharmaceutical firms are not motivated by profit alone, they are motivated by profit. Profit is what large shareholders – hedge funds and other professional investors – care greatly about; and such shareholders have the power to discipline and even to fire non-compliant CEOs and are forever breathing down their necks. It should not be too surprising, then, that, on closer inspection, our experience with the COVID-19 pandemic is uncomfortably close to what would have happened in a world of exclusively profit-maximizing firms.
The COVID-19 Pandemic
 COVID-19 has infected a substantial percentage of humanity. Despite billions of vaccine doses delivered to nearly all countries and territories worldwide, millions of people have either succumbed to the virus or been left with debilitating long-term ailments.
COVID-19 has infected a substantial percentage of humanity. Despite billions of vaccine doses delivered to nearly all countries and territories worldwide, millions of people have either succumbed to the virus or been left with debilitating long-term ailments.
The global surge in numbers affected by this pandemic has triggered R&D of an effective vaccine in record time – under one year as against the previous record of 4 years achieved in the development of the mumps vaccine (Solis-Moreira, 2020). This success is a result of funding by several governments such as that of the United States, where ‘Operation Warp Speed’ was launched, public health agencies like the U.S. Centers for Disease Control, international organizations such as the World Bank and the WHO, and the private sector (Felter, 2021). All of these have played a significant role in expediting vaccine development.
To understand the complex processes involved in producing a vaccine, one must know about such key actors: how much they invested, when and where, into promoting vaccine R&D. This information is critical for understanding the distribution of risks and potential rewards and the influence of R&D investments on who gets early access to its fruits – which in turn can help us think about how to prepare for future epidemics.
The Scramble for Vaccines during the Covid Crisis
Development of a Covid-19 vaccine became a priority for many scientists at numerous pharmaceutical and biotech companies around the world, eager to defeat the pandemic that was holding the world hostage. But this ambition was frustrated as it became apparent that poorer populations would not be included any time soon in the vaccination effort.
Despite COVID-19 being perceived as a ‘rich man’s disease’ or a high-class import that has been carried in by travelers (Bengali, Linthicum and Kim, 2020), the pandemic has grossly affected poorer nations in comparison to their rich counterparts, who in some cases had fewer infections but were the first to receive their doses. According to the Global Health Centre, the U.S. and Germany were the largest investors in vaccine R&D, along with other high-income countries. And while the United Kingdom was the first country to initiate a COVID vaccination drive, the U.S. and Germany were also among the very first countries to gain access to large quantities of the vaccine. Buyers offering greater financial rewards were compensated with early access, even while other countries were facing more dire pandemic conditions.
The suggestion that pharmaceutical companies providing the vaccines were and are still partly driven by profits, is not a hyperbole when one considers which countries have been severely affected by the pandemic through the ‘mismanagement’ of vaccine distribution. An appeal made by the WHO in August 2021 called for a temporary halt in the administration of booster shots for COVID vaccinations in rich countries, due to rates of less than 2% in vaccine distribution in low-income countries in sharp contrast to high-income countries, where over 55% have been fully vaccinated. In a variation of ‘first come first serve,’ those who paid more or early (through financing R&D investment) received priority.
Innovator firms’ public declarations that they would help end the pandemic globally have not been reflected in their distribution policies. They have not provided early vaccine access to countries severely affected by the virus or ones where new disease variants were emerging. Instead, they have practiced ‘buyer favoritism’ and have thereby increased their profits by selling at higher prices and by prolonging the pandemic. They have followed the Friedmanian path.
Scaling Up Vaccine Production Causes a Demand-Supply Imbalance
As the pandemic has continued through several cycles of infections, Big Pharma has recognized the need for rapid mass production of vaccines. Scaling-up vaccine production is an impressive feat for any pharmaceutical company as lack of equipment, cost and time needed for licensing approval, shortage in essential components for the rapid scale-up, and poor strategic distribution of vaccines (Irwin, 2021) have in the past prevented many firms from meeting their production targets. Pfizer and Moderna faced this problem with their commitment to manufacture and deliver 100 million doses at the beginning of the pandemic. In the months leading up to the delivery deadline, they had been steadily producing approximately 4.3 million doses a week instead of the 7.5 million they would have had to deliver to meet their target (Lupkin, 2021). This scaling-up problem could have been solved by involving other firms in vaccine manufacturing on favorable terms. But the patent regime encourages innovators to keep their technologies and know-how to themselves in order to preserve their pricing power and to reduce future competition.
Patents not merely secure the right to market one’s product once it has received marketing approval. They also prevent others from selling the same product and often impede the development and marketing of similar, competing products through what is called strategic patenting (Gurgula, 2020). In this way, patents help capture market share, as exemplified by Pfizer/BioNTech and Moderna vaccines capturing 70% of the total $36.907 billion in sales of COVID-19 Vaccines and Drugs during January-June 2021 (Philippidis, 2021).
Such patenting has not only hampered efforts to curb the spread of the virus but has also obstructed any form of capacity building. This limitation has barred the aiding and provision of innovative approaches to fighting the virus in low-income countries (Linn, 2020) – so much so that the South African and Indian governments have requested that the intellectual property (IP) rights related to COVID-19 be suspended (Usher, 2020). Such a patent waiver would encourage low-income countries to invest in building capacity to manufacture their own affordable vaccines and alleviate the supply chain challenges discussed above. Many are opposed to this proposal, including the Pharmaceutical Research and Manufacturers of America (PhRMA) president and CEO Stephen J. Ubl, who fears that a patent waiver would cause financial loss for many firms.
The numerous issues and challenges that have been outlined thus far concerning pharmaceutical companies and their handling of the pandemic reveal an unfortunate pattern of vulnerable and low-income countries being neglected when firms seek to maximize their profits from markups. Our experience with the COVID-19 pandemic closely parallels what would happen in a Friedmanian world of exclusively profit-maximizing firms. We need a better way of responding to epidemics, one that serves the needs of all.
A Better Approach to Pandemic Threats
 It makes much sense, therefore, to explore whether such firms might perform better against a pandemic threat if they were differently incentivized and rewarded. How differently? The profits of pharmaceutical firms ought to track how well they serve human needs through fast containment and suppression of disease. For this purpose, such firms must solve a three-part task: quickly develop one or more pharmaceuticals that strongly protect from harm not merely treated patients but also third parties whom these patients might infect, quickly expand manufacture to meet – not merely market demand but – all worldwide need for the new pharmaceutical(s), including the needs of the poorest, and then quickly deliver this manufactured supply in a strategic sequence calculated to crush the epidemic as quickly and thoroughly as possible.
It makes much sense, therefore, to explore whether such firms might perform better against a pandemic threat if they were differently incentivized and rewarded. How differently? The profits of pharmaceutical firms ought to track how well they serve human needs through fast containment and suppression of disease. For this purpose, such firms must solve a three-part task: quickly develop one or more pharmaceuticals that strongly protect from harm not merely treated patients but also third parties whom these patients might infect, quickly expand manufacture to meet – not merely market demand but – all worldwide need for the new pharmaceutical(s), including the needs of the poorest, and then quickly deliver this manufactured supply in a strategic sequence calculated to crush the epidemic as quickly and thoroughly as possible.
What kind of reward system might provide optimal incentives to pharmaceutical firms? The most important objective here is to incentivize firms to fully include poor people in their strategy right from the start. For this to happen, an effective new pharmaceutical must be cheap enough to be affordable to all; and delivering it even to the poorest must be profitable enough for firms to be eager to do so comprehensively and effectively. In our world of widespread poverty, these two requirements stand in tension. There is no sales price that is low enough to fulfill the former, and high enough to fulfill the latter requirement. To resolve this tension, firms must receive a delivery premium in addition to the sales price. Such a premium, tied to health gain achieved, is an essential component of the Health Impact Fund approach, which offers firms performance rewards based on the real health gains they achieve with any of their products, on condition that they sell this product without markup.6
Let us explore how this approach might be applied to the special case of vaccinating humankind against a pandemic disease. Here the core idea is to guarantee a reward payment for every indicated vaccination event anywhere. This guaranteed reward payment should be entirely independent of the economic position of the recipients or of their country, and based solely on how vaccinations with a specific vaccine improve the health prospects of the person vaccinated and/or of other persons who might (directly or indirectly) become infected through this person. How large the aggregate health gain from vaccinating some given group of persons is depends then on facts about the vaccine administered, the time of vaccination, the people vaccinated, and their environment, including existing disease vectors.
It would evidently be infeasible to assess the specific health gain achieved by each vaccination event individually. Fortunately, this is not necessary because the objective is not to ascertain the whole causal truth but to provide optimal incentives. For this purpose, reasonable approximations suffice. The reward should be sensitive to the extent to which a vaccination reduces the probability that its recipients will become infected and will infect others, and also sensitive to the extent to which it reduces the harm its recipients will suffer if they become infected despite having been vaccinated. These sensitivities result in a larger payment for vaccinations that are delivered sooner or provide better protection, including protection that works against more variants or remains effective for longer.
These sensitivities also entail higher rewards for delivering vaccinations to persons who are at higher risk of being infected and/or of infecting others – persons in high-incidence countries or regions, for instance, and persons in more interactive professional groups. However, such incentivizing differentiations in the reward per vaccination should be made only insofar as the vaccine provider is in charge of the relevant delivery decisions. If the vaccine supply is allocated by a national health service or by some international organization (such as the WHO or COVAX), then the reward should more simply be based on delivery time and, mainly, on vaccine quality as manifested in its average impact given the general risk level prevailing in the relevant (national, regional or global) delivery population.
In the face of the COVID-19 epidemic, a timely guarantee that the vaccination of every vaccine-eligible person will be amply rewarded would have required a large reward pool, somewhere in the order of $50–100 billion, 0.1–0.2% of the combined gross national incomes of the affluent countries. This is substantially more than the few billions that COVAX has had at its disposal, enabling it to deliver ca. 150–200 million doses thus far, enough for about 100 million immunizations. But then the amount needed to back a universal guarantee is also vastly smaller than the economic damage this pandemic is causing worldwide and the national economic stimulus packages it has triggered, which are valued in the tens of trillions.
The proposed guarantee of universal vaccination would instantly remove any concern about whether vaccinating humanity’s poorer half will be profitable. It would incline competing pharmaceutical innovators to seek to develop a highly effective vaccine and then to ramp up manufacture quickly so as to capture the largest-feasible share of the reward pool. When a firm’s profit margin is essentially fixed, based on its manufacturing costs and the effectiveness of its vaccine, then this firm’s profit depends on speed and quantity, on how many vaccinations are performed with its product. Each firm has an incentive, then, to effect delivery of its product as soon as possible. Firms would compete to use all available manufacturing capacity around the world and also to expand such capacity toward accelerating deliveries.
These desirable incentives would be disturbed if some buyers were offering substantially higher per-dose payments in order to jump the queue. Such offers would cause departures from the optimal vaccination sequence – rich people with low infection risk would be vaccinated before even frontline health workers in poor countries. The prospect of such offers could also undermine the incentive for firms to deliver with maximum speed: slowness of manufacture and delivery prolongs the demand-supply imbalance that encourages and sustains a bidding war among rich buyers. Any such disturbance would make it harder to contain and suppress the pandemic globally, and rich countries ought therefore to subordinate their national interest to the best global strategy by agreeing to draw their vaccines solely from the single vaccine flow created by the global reward pool. In the present pandemic, they have utterly failed to do so. Thus far, about 6% of vaccine doses have been distributed through COVAX and the remaining 94% through a secretive bidding war among affluent buyers. No wonder, then, that the relevant pharmaceutical innovators are in no hurry to ramp up manufacture to immunize the world: potential profits from vaccinating the poorer half are small and doubtful, while large profits beckon from the continued demand-supply imbalance.
Notes
¹ Unicef.org. 2021. COVID-19 Vaccine Market Dashboard. [online] Available at: <https://www.unicef.org/supply/covid-19-vaccine-market-dashboard> [Accessed 31 October 2021].
² Graduate Institute of International and Development Studies. 2021. COVID-19 Vaccine R&D Investments. [online] Available at: <https://www.knowledgeportalia.org/covid19-r-d-funding> [Accessed 3 November 2021].
³ Aljazeera 2021. Which countries have rolled out COVID vaccine?. [online] Available at: <https://www.aljazeera.com/news/2020/12/24/vaccine-rollout-which-countries-have-started> [Accessed 3 November 2021].
⁴ Nature, 2021. The WHO is right to call a temporary halt to COVID vaccine boosters. [online] 596(7872), pp.317-317. Available at: <https://www.nature.com/articles/d41586-021-02219-w> [Accessed 3 November 2021].
⁵ Phrma.org. 2021. PhRMA Statement on WTO TRIPS Intellectual Property Waiver. [online] Available at: <https://www.phrma.org/coronavirus/phrma-statement-on-wto-trips-intellectual-property-waiver> [Accessed 12 November 2021].
6 HealthImpactFund.org. 2021. Health Impact Fund. Delink the Price of Drugs from the Cost of Research. [online] Available at: <https://healthimpactfund.org/en> [Accessed 16 November 2021].
References
Bengali, S., Linthicum, K. and Kim, V., 2020. How Coronavirus – a ‘Rich Man’s Disease’ – Infected the Poor. [online] Los Angeles Times. Available at: <https://www.latimes.com/world-nation/story/2020-05-08/how-the-coronavirus-began-as-a-disease-of-the-rich> [Accessed 12 November 2021].
Felter, C. (2021). A Guide to Global COVID-19 Vaccine Efforts. Council on Foreign Relations. Retrieved 26 July 2021, from https://www.cfr.org/backgrounder/guide-global-covid-19-vaccine-efforts.
Gurgula, O. (2020). Strategic Patenting by Pharmaceutical Companies – Should Competition Law Intervene?. IIC – International Review of Intellectual Property and Competition Law, 51(9), 1062-1085. https://doi.org/10.1007/s40319-020-00985-0
Irwin, A. (2021). What It Will Take to Vaccinate the World against COVID-19. Nature, 592(7853), 176-178. https://doi.org/10.1038/d41586-021-00727-3
Linn, L., 2020. Developing Countries Can Respond to COVID-19 in Ways that are Swift, at Scale, and Successful. [online] Brookings. Available at: <https://www.brookings.edu/blog/future-development/2020/06/04/developing-countries-can-respond-to-covid-19-in-ways-that-are-swift-at-scale-and-successful/> [Accessed 12 November 2021].
Lupkin, S., 2021. Moderna and Pfizer Need to Nearly Double COVID-19 Vaccine Deliveries to Meet Goals. [online] Npr.org. Available at: <https://www.npr.org/sections/health-shots/2021/01/22/959732433/moderna-and-pfizer-need-to-nearly-double-covid-19-vaccine-deliveries-to-meet-goa> [Accessed 12 November 2021].
Maragakis, L., 2021. Coronavirus Second Wave, Third Wave and Beyond: What Causes a COVID Surge. [online] Hopkinsmedicine.org. Available at: <https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/first-and-second-waves-of-coronavirus> [Accessed 11 November 2021].
Philippidis, A., 2021. Top 11 Best Selling COVID-19 Vaccines and Drugs of H1 2021. [online] GEN – Genetic Engineering and Biotechnology News. Available at: <https://www.genengnews.com/a-lists/top-11-best-selling-covid-19-vaccines-and-drugs-of-h1-2021/> [Accessed 3 November 2021].
Solis-Moreira, J., 2020. COVID-19 vaccine: How was It Developed so Fast?. [online] medicalnewstoday.com. Available at: <https://www.medicalnewstoday.com/articles/how-did-we-develop-a-covid-19-vaccine-so-quickly> [Accessed 31 October 2021].
WHO Coronavirus (COVID-19) Dashboard. Covid19.who.int. (2021). Retrieved 25 July 2021, from https://covid19.who.int.
Authors
Zeke Ngcobo received her master’s in public health at Sahmyook University in South Korea. She has launched a website called All Things Public Health that is dedicated to the dissemination of accurate information on matters pertaining to public health. She currently works with the Health Impact Fund as the Regional Coordinator for Sub Saharan Africa.
Having received his PhD in philosophy from Harvard, Thomas Pogge is Leitner Professor of Philosophy and International Affairs and founding Director of the Global Justice Program at Yale. He co-founded Academics Stand Against Poverty, an international network aiming to enhance the impact of scholars, teachers and students on global poverty (www.academicsstand.org), and Incentives for Global Health, a team effort toward creating new incentives that would improve access to advanced pharmaceuticals worldwide (www.healthimpactfund.org). More information athttps://campuspress.yale.edu/thomaspogge/


3 Comments
נערות ליווי
I must thank you for the efforts youve put in penning this site. I am hoping to check out the same high-grade blog posts by you in the future as well. In fact, your creative writing abilities has motivated me to get my very own blog now 😉
דירות דיסקרטיות בחולון
I need to to thank you for this great read!! I certainly loved every bit of it. I have got you book-marked to look at new things you postÖ
Mark
Thanks for your blog, nice to read. Do not stop.